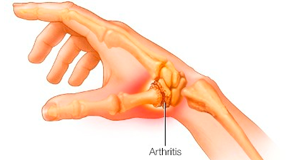
Arthritis
Main symptoms of Arthritis are joint pain and stiffness
Arthritis is the swelling and delicacy of one or more joints. The main symptoms of arthritis are joint pain and stiffness, which commonly increase with age. The most common types of arthritis are osteoarthritis and rheumatoid arthritis.
Severe arthritis, particularly if it affects your hands or arms, can make it difficult for you to do daily tasks. Arthritis of weight-bearing joints can keep you from walking comfortably or sitting up straight. In some cases, joints may gradually lose their alignment and shape.
Shreya Hospital at Ghaziabad is the best Arthritis treatment and diagnosis center in Delhi NCR. Senior Orthopedic Surgeon working at Shreya Hospital have expertise and vast experience in treating Arthritis.
Types of Arthritis:-
Ankylosing Spondylitis
Ankylosing Spondylitis

Ankylosing Spondylitis, also known as axial spondyloarthritis, is an inflammatory disease that, over time, can cause some of the bones in the spine, called vertebrae, to fuse. This fusing makes the spine less flexible and can result in a hunched posture. If ribs are affected, it can be difficult to breathe deeply.
As ankylosing spondylitis worsens, new bone forms as part of the body’s attempt to heal. The new bone gradually bridges the gaps between vertebrae and eventually fuses sections of vertebrae together. Fused vertebrae can flatten the natural curves of the spine, which causes an inflexible, hunched posture.
Symptoms typically begin in early adulthood. Inflammation also can occur in other parts of the body — most commonly, the eyes.
The areas most commonly affected are:
- The joint between the base of the spine and the pelvis.
- The vertebrae in the lower back.
- The places where tendons and ligaments attach to bones, mainly in the spine, but sometimes along the back of the heel.
- The cartilage between the breastbone and the ribs.
- The hip and shoulder joints.
Ankylosing Spondylitis has two types. When the condition is found on X-ray, it is called Ankylosing Spondylitis, also known as Axial Spondyloarthritis. When the condition can’t be seen on X-ray but is found based on symptoms, blood tests and other imaging tests, it is called Non-radiographic Axial Spondyloarthritis.
There is no cure for ankylosing spondylitis, but treatments can lessen symptoms and possibly slow progression of the disease. Medicines can relieve inflammation, pain and stiffness.
Therapy
Physical therapy is an important part of treatment and can provide a number of benefits, from pain relief to improved strength and flexibility. A physical therapist can suggest specific exercises:
- Range-of-motion and stretching exercises.
- Strengthening exercises for abdominal and back muscles.
- Proper sleeping and walking positions.
Surgery may be recommended if you have severe pain or if a hip joint is so damaged that it needs to be replaced.
Gout
Gout
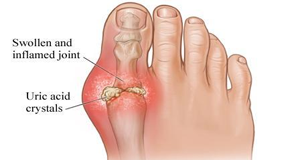
Gout is a common and complex form of arthritis that can affect anyone. It’s characterized by sudden, severe attacks of pain, swelling, redness and tenderness in one or more joints, most often in the big toe.
It occurs when urate crystals accumulate in your joint, causing the inflammation and intense pain of a gout attack. Urate crystals can form when you have high levels of uric acid in your blood. Your body produces uric acid when it breaks down purines. Purines are also found in certain foods, including red meat and organ meats, such as liver. Purine-rich seafood includes anchovies, sardines, mussels, scallops, trout and tuna. Alcoholic beverages, especially beer, and drinks sweetened with fruit sugar (fructose) promote higher levels of uric acid.
Normally, uric acid dissolves in your blood and passes through your kidneys into your urine. But sometimes either your body produces too much uric acid or your kidneys excrete too little uric acid. When this happens, uric acid can build up, forming sharp, needle like urate crystals in a joint or surrounding tissue that cause pain, inflammation and swelling.
Doctors usually diagnose gout based on your symptoms and the appearance of the affected joint. Tests to help diagnose gout include- Joint fluid test, Blood test, X-ray imaging, Ultrasound, Dual-energy computerized tomography (DECT).
Treatment of Gout is available in two types depending on two different problems. The first type helps reduce the inflammation and pain associated with gout attacks. The second type works to prevent gout complications by lowering the amount of uric acid in your blood. Which type of medication is right for you depends on the frequency and severity of your symptoms, along with any other health problems you may have.
Juvenile Idiopathic Arthritis
Juvenile Idiopathic Arthritis

Juvenile Idiopathic Arthritis, formerly known as juvenile rheumatoid arthritis, is the most common type found in children under the age of 16. Juvenile idiopathic arthritis can cause persistent joint pain, swelling, stiffness and some cases high fever.
Some children may experience symptoms for only a few months, while others have symptoms for many years.Some types of juvenile idiopathic arthritis can cause serious complications, such as growth problems, joint damage and eye inflammation. Juvenile idiopathic arthritis occurs when the body’s immune system attacks its own cells and tissues. It’s not known why this happens, but both heredity and environment seem to play a role. Eye problems or growth problem can be found in children due to serious Juvenile idiopathic arthritis.
Diagnosis is difficult and many test like Erythrocyte sedimentation rate (ESR), C-reactive protein, Antinuclear antibody, Rheumatoid factor, Cyclic citrullinated peptide (CCP) can help.
Treatment for juvenile idiopathic arthritis focuses on helping your child maintain a normal level of physical and social activity. To accomplish this, doctors may use a combination of strategies to relieve pain and swelling, maintain full movement and strength, and prevent complications.Treatment focuses on controlling pain and inflammation, improving function, and preventing damage. In very severe cases, surgery may be needed to improve joint function.
Osteoarthritis
Osteoarthritis

Osteoarthritis is the most common form of arthritis, affecting millions of people worldwide. It occurs when the protective cartilage that cushions the ends of the bones wears down over time. Although osteoarthritis can damage any joint, the disorder most commonly affects joints in your hands, knees, hips and spine.
Symptoms of Osteoarthritis include:
- Pain. Affected joints might hurt during or after movement.
- Stiffness. Joint stiffness might be most noticeable upon awakening or after being inactive.
- Tenderness. Your joint might feel tender when you apply light pressure to or near it.
- Loss of flexibility. You might not be able to move your joint through its full range of motion.
- Grating sensation. You might feel a grating sensation when you use the joint, and you might hear popping or crackling.
- Bone spurs. These extra bits of bone, which feel like hard lumps, can form around the affected joint.
- Swelling. This might be caused by soft tissue inflammation around the joint.
It occurs when the cartilage that cushions the ends of bones in your joints gradually deteriorates. Cartilage is a firm, slippery tissue that enables nearly friction less joint motion. Eventually, if the cartilage wears down completely, bone will rub on bone.
Osteoarthritis has often been referred to as a wear and tear disease. But besides the breakdown of cartilage, osteoarthritis affects the entire joint. It causes changes in the bone and deterioration of the connective tissues that hold the joint together and attach muscle to bone. It also causes inflammation of the joint lining.
Risk Factors of osteoarthritis include:
- Older age. The risk of osteoarthritis increases with age.
- Sex. Women are more likely to develop osteoarthritis, though it isn’t clear why.
- Obesity. Carrying extra body weight contributes to osteoarthritis in several ways, and the more you weigh, the greater your risk. Increased weight adds stress to weight-bearing joints, such as your hips and knees. Also, fat tissue produces proteins that can cause harmful inflammation in and around your joints.
- Joint injuries. Injuries, such as those that occur when playing sports or from an accident, can increase the risk of osteoarthritis. Even injuries that occurred many years ago and seemingly healed can increase your risk of osteoarthritis.
- Repeated stress on the joint. If your job or a sport you play places repetitive stress on a joint, that joint might eventually develop osteoarthritis.
- Genetics. Some people inherit a tendency to develop osteoarthritis.
- Bone deformities. Some people are born with malformed joints or defective cartilage.
- Certain metabolic diseases. These include diabetes and a condition in which your body has too much iron.
Osteoarthritis is a degenerative disease that worsens over time, often resulting in chronic pain. Joint pain and stiffness can become severe enough to make daily tasks difficult.
Diagnosis of Osteoarthriti include X-rays, Magnetic resonance imaging (MRI), Blood tests and Joint fluid analysis.
Symptoms can usually be managed, although the damage to joints can’t be reversed. Staying active, maintaining a healthy weight and receiving certain treatments might slow progression of the disease and help improve pain and joint function. Treatments can reduce pain and help you move better.
Treatment of Osteoarthritis vary according to the condition of the patient:
Medications
Medications that can help relieve osteoarthritis symptoms, primarily pain, include:
- Acetaminophen. Acetaminophen (Tylenol, others) has been shown to help some people with osteoarthritis who have mild to moderate pain. Taking more than the recommended dose of acetaminophen can cause liver damage.
- Nonsteroidal anti-inflammatory drugs (NSAIDs). Over-the-counter nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen (Advil, Motrin IB, others) and naproxen sodium (Aleve), taken at the recommended doses, typically relieve osteoarthritis pain. Stronger NSAIDs are available by prescription.NSAIDs can cause stomach upset, cardiovascular problems, bleeding problems, and liver and kidney damage. NSAIDs as gels, applied to the skin over the affected joint, have fewer side effects and may relieve pain just as well.
- Duloxetine (Cymbalta). Normally used as an antidepressant, this medication is also approved to treat chronic pain, including osteoarthritis pain.
Therapy
- Physical therapy. A physical therapist can show you exercises to strengthen the muscles around your joint, increase your flexibility and reduce pain. Regular gentle exercise that you do on your own, such as swimming or walking, can be equally effective.
- Occupational therapy. An occupational therapist can help you discover ways to do everyday tasks without putting extra stress on your already painful joint. For instance, a toothbrush with a large grip could make brushing your teeth easier if you have osteoarthritis in your hands. A bench in your shower could help relieve the pain of standing if you have knee osteoarthritis.
- Transcutaneous electrical nerve stimulation (TENS). This uses a low-voltage electrical current to relieve pain. It provides short-term relief for some people with knee and hip osteoarthritis.
Surgical and other procedures
If medication and Therapy treatments don’t help, doctor might prescribe procedures such as:
- Cortisone injections. Injections of a corticosteroid into your joint might relieve pain for a few weeks. Your doctor numbs the area around your joint, then places a needle into the space within your joint and injects medication. The number of cortisone injections you can receive each year is generally limited to three or four, because the medication can worsen joint damage over time.
- Lubrication injections. Injections of hyaluronic acid might relieve pain by providing some cushioning in your knee, though some research suggests that these injections offer no more relief than a placebo. Hyaluronic acid is similar to a component normally found in your joint fluid.
- Realigning bones. If osteoarthritis has damaged one side of your knee more than the other, an osteotomy might be helpful. In a knee osteotomy, a surgeon cuts across the bone either above or below the knee, and then removes or adds a wedge of bone. This shifts your body weight away from the worn-out part of your knee.
- Joint replacement. In joint replacement surgery, your surgeon removes your damaged joint surfaces and replaces them with plastic and metal parts. Surgical risks include infections and blood clots. Artificial joints can wear out or come loose and might eventually need to be replaced.
Psoriatic Arthritis
Psoriatic Arthritis

Psoriatic Arthritis is a form of arthritis that affects some people who have psoriasis — a disease that causes red patches of skin topped with silvery scales. Most people develop psoriasis years before being diagnosed with psoriatic arthritis. But for some, the joint problems begin before skin patches appear or at the same time.
It can affect joints on one or both sides of your body. The signs and symptoms of psoriatic arthritis often resemble those of rheumatoid arthritis. Both diseases cause joints to become painful, swollen and warm to the touch.
Sometimes It Cause:
- Swollen fingers and toes. Psoriatic arthritis can cause a painful, sausage-like swelling of your fingers and toes.
- Foot pain. Psoriatic arthritis can also cause pain at the points where tendons and ligaments attach to your bones — especially at the back of your heel (Achilles tendinitis) or in the sole of your foot (plantar fasciitis).
- Lower back pain. Some people develop a condition called spondylitis as a result of psoriatic arthritis. Spondylitis mainly causes inflammation of the joints between the vertebrae of your spine and in the joints between your spine and pelvis (sacroiliitis).
- Nail changes. Nails can form tiny dents (pits), crumble or separate from the nail beds.
- Eye inflammation. Uveitis can cause eye pain, redness and blurry vision. If untreated, uveitis can lead to vision loss.
- High Risk health problems like hypertension, metabolic syndrome, diabetes and cardiovascular disease can occur .
Causes:
Psoriatic arthritis occurs when your body’s immune system attacks healthy cells and tissue. The immune response causes inflammation in your joints as well as overproduction of skin cells.
It seems likely that both genetic and environmental factors play a role in this immune system response. Many people with psoriatic arthritis have a family history of either psoriasis or psoriatic arthritis. Researchers have discovered certain genetic markers that appear to be associated with psoriatic arthritis.
Physical trauma or something in the environment — such as a viral or bacterial infection — might trigger psoriatic arthritis in people with an inherited tendency.
Treatment:
No cure exists for Psoriatic Arthritis. Treatment focuses on controlling inflammation in your affected joints to prevent joint pain and disability and controlling skin involvement. One of the most common treatments are prescription medications called disease-modifying antirheumatic drugs (DMARDs).
Treatment will depend on how severe your disease is and what joints are affected. You might have to try different treatments before you find one that brings you relief.
Medications
Drugs used to treat Psoriatic Arthritis include:
- NSAIDs. Nonsteroidal anti-inflammatory drugs (NSAIDs) can relieve pain and reduce inflammation for people with mild psoriatic arthritis. nonsteroidal anti-inflammatory drugs (NSAIDs) available without a prescription include ibuprofen (Advil, Motrin IB, others) and naproxen sodium (Aleve). Stronger NSAIDs are available by prescription. Side effects can include stomach irritation, heart problems, and liver and kidney damage.
- Conventional disease-modifying antirheumatic drugs (DMARDs). These drugs can slow the progression of psoriatic arthritis and save joints and other tissues from permanent damage.The most commonly used disease-modifying antirheumatic drug (DMARD) is methotrexate (Trexall, Otrexup, others). Others include leflunomide (Arava) and sulfasalazine (Azulfidine). Side effects can include liver damage, bone marrow suppression, and lung inflammation and scarring (fibrosis).
- Biologic agents. Also known as biologic response modifiers, this class of DMARD targets different pathways of the immune system. Biologic agents include adalimumab (Humira), certolizumab (Cimzia), etanercept (Enbrel), golimumab (Simponi), infliximab (Remicade), ustekinumab (Stelara), secukinumab (Cosentyx), ixekizumab (Taltz), guselkumab (Tremfya) and abatacept (Orencia). These drugs can increase the risk of infections.
- Targeted synthetic DMARDs. Tofacitinib (Xeljanz) might be used if conventional DMARDs and biologic agents haven’t been effective. Higher doses of tofacitinib can increase the risk of blood clots in the lungs, serious heart-related events and cancer.
- Newer oral medication. Apremilast (Otezla) decreases the activity of an enzyme in the body that controls the activity of inflammation within cells. Apremilast is used for people with mild to moderate psoriatic arthritis who do not want or cannot be treated with DMARDs or biologic agents. Potential side effects include diarrhea, nausea and headaches.
Therapies
Physical and occupational therapies might ease pain and make it easier to do everyday tasks. Ask your doctor for referrals. Massage therapy might also offer relief.
Surgical and other procedures
- Steroid injections. Injections into an affected joint can reduce inflammation.
- Joint replacement surgery. Some joints that have been severely damaged by psoriatic arthritis can be replaced with artificial ones made of metal and plastic.
Reactive Arthritis
Reactive Arthritis
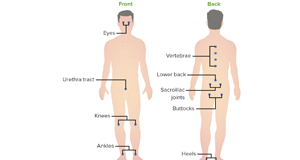
It is joint pain and swelling triggered by an infection in another part of the body — most often the intestines, genitals or urinary tract.
This condition usually targets the knees, ankles and feet. Inflammation also can affect the eyes, skin and the tube that carries urine out of the body (urethra). Previously, reactive arthritis was sometimes called Reiter’s syndrome.
Symptoms
The signs and symptoms of reactive arthritis generally start 1 to 4 weeks after exposure to a triggering infection. They might include:
- Pain and stiffness. The joint pain associated with reactive arthritis most commonly occurs in the knees, ankles and feet. Pain may also occur in the heels, low back or buttocks.
- Eye inflammation. Many people who have reactive arthritis also develop eye inflammation (conjunctivitis).
- Urinary problems. Increased frequency and discomfort during urination may occur, as can inflammation of the prostate gland or cervix.
- Inflammation of tendons and ligaments where they attach to bone (enthesitis). This happens most often in the heels and the sole of the feet.
- Swollen toes or fingers. In some cases, toes or fingers might become so swollen that they look like sausages.
- Skin problems. Reactive arthritis can affect skin in a variety of ways, including mouth sores and a rash on the soles of the feet and palms of the hands.
- Low back pain. The pain tends to be worse at night or in the morning.
Causes:
Reactive arthritis develops in reaction to an infection in your body, often in your intestines, genitals or urinary tract. You might not be aware of the triggering infection if it causes mild symptoms or none at all. Numerous bacteria can cause reactive arthritis. Some are transmitted sexually, and others are foodborne.
The most common bacteria include:
- Campylobacter
- Chlamydia
- Clostridioides difficile
- Escherichia coli
- Salmonella
- Shigella
- Yersinia
Prevention:
Genetic factors appear to play a role in whether you’re likely to develop reactive arthritis. Though you can’t change your genetic makeup, you can reduce your exposure to the bacteria that may lead to reactive arthritis.
Store your food at proper temperatures and cook it properly. Doing these things help you avoid the many foodborne bacteria that can cause reactive arthritis, including salmonella, shigella, yersinia and campylobacter. Some sexually transmitted infections can trigger reactive arthritis. Use condoms to help lower your risk.
Diagnosis:
Blood tests
Your doctor might recommend that a sample of your blood be tested for:
- Evidence of past or current infection
- Signs of inflammation
- Antibodies associated with other types of arthritis
- A genetic marker linked to reactive arthritis
Joint fluid tests
Your doctor might use a needle to withdraw a sample of fluid from within an affected joint. This fluid will be tested for:
- White blood cell count. An increased number of white blood cells might indicate inflammation or an infection.
- Infections. Bacteria in your joint fluid might indicate septic arthritis, which can result in severe joint damage.
- Crystals. Uric acid crystals in your joint fluid might indicate gout. This very painful type of arthritis often affects the big toe.
Imaging tests
X-rays of your low back, pelvis and joints can indicate whether you have any of the characteristic signs of reactive arthritis.
Treatment
The goal of treatment is to manage your symptoms and treat an infection that could still be present.
Medications
If your reactive arthritis was triggered by a bacterial infection, your doctor might prescribe an antibiotic if there is evidence of persistent infection. Which antibiotic you take depends on the bacteria that are present.
Signs and symptoms of reactive arthritis may be eased with:
- Nonsteroidal anti-inflammatory drugs (NSAIDs). Prescription nonsteroidal anti-inflammatory drugs (NSAIDs), such as indomethacin (Indocin), can relieve the inflammation and pain of reactive arthritis.
- Steroids. A steroid injection into affected joints can reduce inflammation and allow you to return to your usual activity level. Steroid eye drops may be used for eye symptoms, and steroid creams might be used for skin rashes.
- Rheumatoid arthritis drugs. Limited evidence suggests that medications such as sulfasalazine (Azulfidine), methotrexate (Trexall) or etanercept (Enbrel) can relieve pain and stiffness for some people with reactive arthritis.
Physical therapy
A physical therapist can provide you with targeted exercises for your joints and muscles. Strengthening exercises increase the joint’s support by developing the muscles around the affected joints. Range-of-motion exercises can increase your joints’ flexibility and reduce stiffness.
Rheumatoid Arthritis
Rheumatoid Arthritis

It is a disorder that can affect not only your joints but can damage other parts of the body as well. Rheumatoid arthritis is an autoimmune disease. Normally, your immune system helps protect your body from infection and disease.
In rheumatoid arthritis, your immune system attacks healthy tissue in your joints. Except joints other parts of the body like Skin, Eyes, Lungs, Heart, Kidneys, Salivary glands, Nerve tissue, Bone marrow and Blood vessels also get affected.
Symptoms of rheumatoid arthritis include Tender, warm, swollen joints, Joint stiffness mostly in the morning, weakness, fever and loss of appetite. In the beginning it affects smaller joints like fingers, hands, toes and foots. And with the time it affects other joints like wrists, knees, ankles, elbows, hips and shoulders. In most cases, symptoms occur in the same joints on both sides of your body.
Rheumatoid arthritis increases your risk of developing:
- Osteoporosis. Rheumatoid arthritis itself, along with some medications used for treating rheumatoid arthritis, can increase your risk of osteoporosis — a condition that weakens your bones and makes them more prone to fracture.
- Rheumatoid nodules. These firm bumps of tissue most commonly form around pressure points, such as the elbows. However, these nodules can form anywhere in the body, including the heart and lungs.
- Dry eyes and mouth. People who have rheumatoid arthritis are much more likely to develop Sjogren’s syndrome, a disorder that decreases the amount of moisture in the eyes and mouth.
- Infections. Rheumatoid arthritis itself and many of the medications used to combat it can impair the immune system, leading to increased infections. Protect yourself with vaccinations to prevent diseases such as influenza, pneumonia, shingles and COVID-19.
- Abnormal body composition. The proportion of fat to lean mass is often higher in people who have rheumatoid arthritis, even in those who have a normal body mass index (BMI).
- Carpal tunnel syndrome. If rheumatoid arthritis affects your wrists, the inflammation can compress the nerve that serves most of your hand and fingers.
- Heart problems. Rheumatoid arthritis can increase your risk of hardened and blocked arteries, as well as inflammation of the sac that encloses your heart.
- Lung disease. People with rheumatoid arthritis have an increased risk of inflammation and scarring of the lung tissues, which can lead to progressive shortness of breath.
- Lymphoma. Rheumatoid arthritis increases the risk of lymphoma, a group of blood cancers that develop in the lymph system.
Diagnosis:
In the early stages of Rheumatoid Arthritis doctor will do physical exam checking joints for swelling, redness and warmth. In some cases doctor might suggest X-Ray to find out the progression of the desease. MRI or Ultrasound can be required to help your doctor judge the severity of the disease in your body.
Treatment:
The types of medications recommended by your doctor will depend on the severity and duration of your symptom.
- NSAIDs. Nonsteroidal anti-inflammatory drugs (NSAIDs) can relieve pain and reduce inflammation. Stronger NSAIDs are available by prescription. Side effects may include stomach irritation, heart problems and kidney damage.
- Steroids. Corticosteroid medications, such as prednisone, reduce inflammation and pain and slow joint damage. Side effects may include thinning of bones, weight gain and diabetes.
- Conventional DMARDs. These drugs can slow the progression of rheumatoid arthritis and save the joints and other tissues from permanent damage. Side effects vary but may include liver damage and severe lung infections.
- Biologic agents. Also known as biologic response modifiers. Biologic DMARDs are usually most effective when paired with a conventional DMARD, such as methotrexate. This type of drug also increases the risk of infections.
- Targeted synthetic DMARDs. Baricitinib (Olumiant), tofacitinib (Xeljanz) and upadacitinib (Rinvoq) may be used if conventional DMARDs and biologics haven’t been effective. Higher doses of tofacitinib can increase the risk of blood clots in the lungs, serious heart-related events and cancer.
Therapy:
A Physical Therapist can teach you exercises to help keep your joints flexible. The therapist may also suggest new ways to do daily tasks that will be easier on your joints. For example, you may want to pick up an object using your forearms.
Assistive devices can make it easier to avoid stressing your painful joints. For instance, a kitchen knife equipped with a hand grip helps protect your finger and wrist joints. Certain tools, such as buttonhooks, can make it easier to get dressed.
Surgery:
If medications fail to prevent or slow joint damage, your doctor may consider surgery to repair damaged joints. Surgery may help restore your ability to use your joint. It can also reduce pain and improve function.
Rheumatoid Arthritis Surgery may involve one or more of the following procedures:
- Synovectomy. Surgery to remove the inflamed lining of the joint (synovium) can help reduce pain and improve the joint’s flexibility.
- Tendon repair. Inflammation and joint damage may cause tendons around your joint to loosen or rupture. Your surgeon may be able to repair the tendons around your joint.
- Joint fusion. Surgically fusing a joint may be recommended to stabilize or realign a joint and for pain relief when a joint replacement isn’t an option.
- Total joint replacement. During joint replacement surgery, your surgeon removes the damaged parts of your joint and inserts a prosthesis made of metal and plastic.
Surgery carries a risk of bleeding, infection and pain. You should discuss the benefits and risks with your doctor.
Septic Arthritis
Septic Arthritis
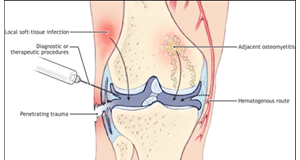
It is a painful infection in a joint that can come from germs that travel through your bloodstream from another part of your body. Septic arthritis can also occur when a penetrating injury, such as an animal bite or trauma, delivers germs directly into the joint.
Infants and older adults are most likely to develop septic arthritis. People who have artificial joints are also at risk of septic arthritis. Knees are most commonly affected, but septic arthritis also can affect hips, shoulders and other joints. The infection can quickly and severely damage the cartilage and bone within the joint, so prompt treatment is crucial.
Septic arthritis typically causes extreme discomfort and difficulty using the affected joint. The joint could be swollen, red and warm, and you might have a fever. Septic arthritis can be caused by bacterial, viral or fungal infections. Septic arthritis can develop when an infection, such as a skin infection or urinary tract infection, spreads through your bloodstream to a joint. Less commonly, a puncture wound, drug injection, or surgery in or near a joint — including joint replacement surgery — can give the germs entry into the joint space.
Diagnosis:
The following tests typically help diagnose septic arthritis:
- Joint fluid analysis. Infections can alter the color, consistency, volume and makeup of the fluid within your joints. A sample of this fluid can be withdrawn from your affected joint with a needle. Laboratory tests can determine what organism is causing your infection, so your doctor will know which medications to prescribe.
- Blood tests. These can determine if there are signs of infection in your blood. A sample of your blood is removed from a vein with a needle.
- Imaging tests. X-rays and other imaging tests of the affected joint can assess damage to the joint or loosening of an artificial joint.
- A Specialized Scan that involves swallowing or injecting a small amount of a radioactive chemical may be used if your doctor suspects you have a prosthetic joint infection and it’s been more than a year since you’ve had surgery.
Treatment:
Doctors rely on joint drainage and antibiotic drugs to treat Septic Arthritis.
Joint Drainage
Removing the infected joint fluid is crucial. Drainage methods include:
- Needle. In some cases, your doctor can withdraw the infected fluid with a needle inserted into the joint space.
- Scope procedure. In arthroscopy (ahr-THROS-kuh-pee), a flexible tube with a video camera at its tip is placed in your joint through a small incision. Suction and drainage tubes are then inserted through small incisions around your joint.
- Open surgery. Some joints, such as the hip, are more difficult to drain with a needle or arthroscopy, so an open surgical procedure might be necessary.
Antibiotics
To select the most effective medication, your doctor must identify the microbe causing your infection. Antibiotics are usually given through a vein in your arm at first. Later, you may be able to switch to oral antibiotics.
Removal of replacement joint
If an artificial joint is infected, treatment often involves removing the joint and temporarily replacing it with a joint spacer — a device made with antibiotic cement. Several months later, a new replacement joint is implanted.
Thumb Arthritis
Thumb Arthritis
This generally occurs with age. Previous trauma or injury to the thumb joint also can cause thumb arthritis. In a normal thumb joint, cartilage covers the ends of the bones — acting as a cushion and allowing the bones to glide smoothly against each other. With thumb arthritis, the cartilage that covers the ends of the bones deteriorates, and its smooth surface roughens. The bones then rub against each other, resulting in friction and joint damage.
The damage to the joint might result in growth of new bone along the sides of the existing bone (bone spurs), which can produce noticeable lumps on your thumb joint. Thumb arthritis can cause severe pain, swelling, and decreased strength and range of motion, making it difficult to do simple tasks, such as turning doorknobs and opening jars.
Physical examination by the Doctor and if require X-Rays being done for the diagnosis of Thumb arthritis.
Treatment
In the early stages of thumb arthritis, treatment usually involves a combination of non-surgical therapies like taking Pain Reliever Tablets and Pain Reliever Lotions to apply on the affected areas. Pain Reliever Injections can also be taken for quicker relief.
Using splint can support your joint and limit the movement of your thumb and wrist. You might wear a splint just at night or throughout the day and night.
If the patient is not getting relief from above treatments or if you’re barely able to bend and twist your thumb, your doctor might recommend surgery.
Surgery include procedures:
- Joint fusion (arthrodesis). The bones in the affected joint are permanently fused. The fused joint can bear weight without pain, but has no flexibility.
- Osteotomy. The bones in the affected joint are repositioned to help correct deformities.
- Trapeziectomy. One of the bones in your thumb joint (trapezium) is removed.
- Joint replacement (arthroplasty). All or part of the affected joint is removed and replaced with a graft from one of your tendons.
After surgery, you can expect to wear a cast or splint over your thumb and wrist for up to six weeks. Once the cast is removed, you might have physical therapy to help you regain hand strength and movement.
 Dr Dev Mishra Best Orthopaedic Doctor in Delhi NCR Ghaziabad
Dr Dev Mishra Best Orthopaedic Doctor in Delhi NCR Ghaziabad