Orthopaedic Treatments
Orthopaedic Treatments for all Skeletal Deformities
Dr Dev Mishra Specialist of Orthopaedic Treatments in ghaziabad. He is Senior Orthopaedic Surgeon with immense experience of more than 20+ Years. He is a popular and experienced Orthopaedic Doctor in Ghaziabad and Delhi, NCR. Dr Dev Mishra is providing services as Senior Orthopedic Specialist at Shreya Hospital the must trusted Healthcare Centre for Orthopaedic Treatments in Ghaziabad.
Our Orthopedic Specialists provide best Orthopaedic Treatments for all kind of Skeletal Deformities, Fractures, Bone Problems,Ligaments, Joint Problems, Arthritis etc. We analyze the issue of our patients using advance surgical equipment and latest diagnosis technologies. All type of everyday bone and joint problems treated with special care and attention. The team of Orthopedic Specialists work relentlessly to build success stories with there experience and expertise in the era of Orthopaedic Treatments.
Experts in all Orthopaedic Treatments:-
Broken Bones & Fractures
Broken Bones & Fractures
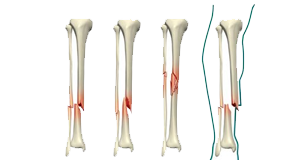
Orthopaedic Treatments, Fracture is the medical term for a broken bone
A bone fracture is the medical definition for a broken bone. Broken Bones and Fractures are a very common injury and can affect anyone at all age. Fractures are usually caused by traumas like falls, car accidents or sports injuries. But some medical conditions and repetitive forces (like running) can increase your risk for experiencing certain types of fractures.
Broken Bones and Fractures are the same injury and mean the same thing. A fracture is the medical term for a broken bone, so your Orthopedic Specialist will probably refer to your broken bone as a certain type of fracture after they diagnose it. Shreya Hospital at Ghaziabad is the best treatment center for Broken Bones and Fractures.
If you break a bone, you might need surgery to repair it. Some people only need a splint, cast, brace or sling for their bone to heal. How long it takes to recover fully depends on which of your bones are fractured, where the fracture is and what caused it.
Different Types of Broken Bones and Fractures need Orthopaedic Treatments:
There are many different types of fractures. Your provider will diagnose a specific fracture type depending on a few criteria, including its:
- Pattern: A fracture pattern is the medical term for the shape of a break or what it looks like.
- Cause: Some fractures are classified by how they happen.
- Body part: Where in your body your broke a bone.
Diagnosed by pattern or shape
Some fractures are classified by their pattern. This can either be the direction a break goes (if it’s a straight light across your bone) or its shape (if it’s more than a single line break).
Fractures that have a single straight-line break include:
- Oblique fractures.
- Transverse fractures.
- Longitudinal fractures (breaks that happen along the length of the bone).
Fracture patterns that don’t break your bone in a single straight line include:
- Greenstick fractures.
- Comminuted fractures.
- Segmental fractures.
- Spiral fractures.
Diagnosed by cause
A few types of fractures are named or classified by what causes them. These include:
- Stress fractures (sometimes referred to as hairline fractures).
- Avulsion fractures.
- Buckle fractures (sometimes referred to as torus or impacted fractures).
Diagnosed by location
Lots of fractures are specific to where they happen in your body. In some cases, it’s possible to experience a location-based fracture that’s also one of the other types listed above. For example, someone who experiences a severe fall might have a comminuted tibia (shin bone) fracture.
Fractures that affect people’s chest, arms and upper body include:
- Clavicle fractures (broken collarbones).
- Shoulder fractures.
- Humerus (upper arm bone) fractures.
- Elbow fractures.
- Rib fractures.
- Compression fractures.
- Facial fractures.
Some fractures that can affect your hands or wrists include:
- Barton fractures.
- Chauffeur fractures.
- Colles fractures.
- Smith fractures.
- Scaphoid fractures.
- Metacarpal fractures (breaking any of the bones in your hand that connect your wrist to your fingers).
Fractures that damage the bones in your lower body and legs include:
- Pelvic fractures.
- Acetabular fractures.
- Hip fractures.
- Femur fractures.
- Patella fractures.
- Growth plate fractures.
- Tibia (your shin bone) and fibula (your calf bone) fractures.
Fractures that affect your feet and ankles are more likely to have complications like nonunion. They include:
- Calcaneal stress fractures.
- Fifth metatarsal fractures.
- Jones fractures.
- Lisfranc fractures.
- Talus fractures.
- Trimalleolar fractures.
- Pilon fractures.
Back Pain Problem
Back Pain Problem
Orthopaedic Treatments for Back Pain Problem

Back Pain is a leading cause of disability worldwide.
Back pain is one of the most common reasons people seek medical help. Sometimes it becomes difficult to work due to sever Back pain. It is a leading cause of disability worldwide.
Causes:
Causes commonly linked to back pain include:
- Muscle or ligament strain. Repeated heavy lifting or a sudden awkward movement can strain back muscles and spinal ligaments. For people in poor physical condition, constant strain on the back can cause painful muscle spasms.
- Bulging or ruptured disks. Disks act as cushions between the bones in the spine. The soft material inside a disk can bulge or rupture and press on a nerve. However, a bulging or ruptured disk might not cause back pain. Disk disease is often found on spine X-rays, CT scans or MRIs done for another reason.
- Arthritis. Osteoarthritis can affect the lower back. In some cases, arthritis in the spine can lead to a narrowing of the space around the spinal cord, a condition called spinal stenosis.
- Osteoporosis. The spine’s vertebrae can develop painful breaks if the bones become porous and brittle.
- Ankylosing spondylitis, also called axial spondyloarthritis. This inflammatory disease can cause some of the bones in the spine to fuse. This makes the spine less flexible.
Back Pain is common among all age groups, even children.
These factors can increase the risk of developing back pain:
- Age. Back pain is more common with age, starting around age 30 or 40.
- Lack of exercise. Weak, unused muscles in the back and abdomen might lead to back pain.
- Excess weight. Excess body weight puts extra stress on the back.
- Diseases. Some types of arthritis and cancer can contribute to back pain.
- Improper lifting. Using the back instead of the legs can lead to back pain.
- Psychological conditions. People prone to depression and anxiety appear to have a greater risk of back pain. Stress can cause muscle tension, which can contribute to back pain.
- Smoking. Smokers have increased rates of back pain. This may occur because smoking causes coughing, which can lead to herniated disks. Smoking also can decrease blood flow to the spine and increase the risk of osteoporosis.
Orthopedic Specialist at Shreya Hospital, Ghaziabadwill examine your back and assess your ability to sit, stand, walk and lift your legs. Doctor might ask you about how your pain affects your daily activities. It helps in the diagnosis of Back Pain. You might be asked to follow some tests like:
- X-ray. These images show arthritis or broken bones. These images alone won’t show problems with the spinal cord, muscles, nerves or disks.
- MRI or CT scans. These scans generate images that can reveal herniated disks or problems with bones, muscles, tissue, tendons, nerves, ligaments and blood vessels.
- Blood tests. These can help determine whether an infection or other condition might be causing pain.
- Nerve studies. Electromyography (EMG) measures the electrical impulses produced by the nerves and how the muscles respond to them. This test can confirm pressure on the nerves caused by herniated disks or narrowing of the spinal canal (spinal stenosis).
Orthopaedic Treatments
Most back pain gets better within a month of home treatment, especially for people younger than age 60. However, for many, the pain lasts long. Pain relievers and the use of heat might be all that’s needed.
Continue your activities as much as you can with back pain. Try light activity, such as walking. Stop activity that increases pain, but don’t avoid activity out of fear of pain. If home treatments aren’t working after several weeks, your doctor might recommend medications or other therapies.
Medications
Medications depend on the type of back pain. They might include:
- Pain relievers. Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen (Advil, Motrin IB, others) or naproxen sodium (Aleve), might help. Take these medications only as directed. Overuse can cause serious side effects. If pain relievers you can buy without a prescription don’t help, your health care provider might suggest prescription NSAIDs.
- Muscle relaxants. If mild to moderate back pain doesn’t improve with pain relievers, a muscle relaxant might help. Muscle relaxants can cause dizziness and sleepiness.
- Topical pain relievers. These products, including creams, salves, ointments and patches, deliver pain-relieving substances through the skin.
- Narcotics. Drugs containing opioids, such as oxycodone or hydrocodone, may be used for a short time with close medical supervision.
- Antidepressants. Some types of antidepressants — particularly duloxetine (Cymbalta) and tricyclic antidepressants, such as amitriptyline — have been shown to relieve chronic back pain.
Physical therapy
A physical therapist can teach exercises to increase flexibility, strengthen back and abdominal muscles, and improve posture. Regular use of these techniques can stop recurring of Back Pain.
Surgical and other procedures
Procedures used to treat back pain may include:
- Cortisone injections. If other measures don’t relieve pain that radiates down the leg, an injection of cortisone plus a numbing medication into the space around the spinal cord and nerve roots might help. A cortisone injection helps decrease inflammation around the nerve roots, but the pain relief usually lasts only a month or two.
- Radiofrequency ablation. In this procedure, a fine needle is inserted through skin near the area causing the pain. Radio waves are passed through the needle to damage the nearby nerves. Damaging the nerves interferes with pain signals to the brain.
- Implanted nerve stimulators. Devices implanted under the skin can deliver electrical impulses to certain nerves to block pain signals.
- Surgery. Surgery to create more space within the spine is sometimes helpful for people who have increasing muscle weakness or back pain that goes down a leg. These problems can be related to herniated disks or other conditions that narrow the openings within the spine.
Arthritis
Arthritis
Orthopaedic Treatments for Arthritis
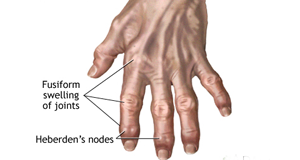
Main symptoms of Arthritis are joint pain and stiffness
Arthritis is the swelling and delicacy of one or more joints. The main symptoms of arthritis are joint pain and stiffness, which commonly increase with age. The most common types of arthritis are osteoarthritis and rheumatoid arthritis.
Severe arthritis, particularly if it affects your hands or arms, can make it difficult for you to do daily tasks. Arthritis of weight-bearing joints can keep you from walking comfortably or sitting up straight. In some cases, joints may gradually lose their alignment and shape.
Shreya Hospital at Ghaziabad is the best Arthritis treatment and diagnosis center in Delhi NCR. Senior Orthopedic Surgeon working at Shreya Hospital have expertise and vast experience in treating Arthritis.
Types of Arthritis:-
-
Ankylosing Spondylitis
-
Gout
-
Juvenile Idiopathic Arthritis
-
Osteoarthritis
-
Psoriatic Arthritis
-
Reactive Arthritis
-
Rheumatoid Arthritis
-
Septic Arthritis
-
Thumb Arthritis
Muscles Strain and Sprain
Muscles Strain and Sprain
Orthopaedic Treatments for Muscles Strain and Sprain

Orthopaedic Treatments for Muscles Strain
A muscle strain is an injury to a muscle or a tendon — the fibrous tissue that connects muscles to bones. Minor injuries may only overstretch a muscle or tendon, while more severe injuries may involve partial or complete tears in these tissues. Sometimes called pulled muscles, strains commonly occur in the lower back and in the muscles at the back of the thigh (hamstrings).
The difference between a strain and a sprain is that a strain involves an injury to a muscle or to the band of tissue that attaches a muscle to a bone, while a sprain injures the bands of tissue that connect two bones together.
Symptoms
Symptoms will vary, depending on the severity of the injury, and may include:
- Pain or tenderness
- Redness or bruising
- Limited motion
- Muscle spasms
- Swelling
- Muscle weakness
Causes
Muscle Strains can be caused by one event, such as using poor body mechanics to lift something heavy. Chronic muscle strains can result from repetitive injuries when you stress a muscle by doing the same motion over and over.
Risk factors
Participating in sports such as soccer, football, hockey, boxing and wrestling can increase your risk of muscle strains.
Certain parts of the body are more susceptible to strains during participation in certain sports. May include:
- Legs and ankles. Sports that feature quick starts and jumping, such as hurdling and basketball, can be particularly tough on the Achilles tendon in your ankle.
- Hands. Gripping sports, such as gymnastics or golf, can increase your risk of muscle strains in your hands.
- Elbows. Elbow strains are often caused by throwing sports and racquet sports.
Diagnosis
During the physical exam, your doctor will check for swelling and points of tenderness. The location and intensity of your pain can help determine the extent and nature of the damage.
In more severe injuries, where the muscle or tendon has been completely ruptured, your doctor may be able to see or feel a defect in the area of injury. Ultrasound can help to find out the injuries.
Orthopaedic Treatments
Orthopedic Specialist working at Shreya Hospital, Ghaziabad can guide you for immediate self-care of a muscle strain, try the R.I.C.E. approach — rest, ice, compression, elevation:
- Rest. Avoid activities that cause pain, swelling or discomfort. But don’t avoid all physical activity.
- Ice. Even if you’re seeking medical help, ice the area immediately. Use an ice pack or slush bath of ice and water for 15 to 20 minutes each time and repeat every two to three hours while you’re awake for the first few days after the injury.
- Compression. To help stop swelling, compress the area with an elastic bandage until the swelling stops. Don’t wrap it too tightly or you may hinder circulation. Begin wrapping at the end farthest from your heart. Loosen the wrap if the pain increases, the area becomes numb or swelling is occurring below the wrapped area.
- Elevation. Elevate the injured area above the level of your heart, especially at night, which allows gravity to help reduce swelling.
A physical therapist can help you to maximize stability and strength of the injured joint or limb. Your doctor may suggest that you immobilize the area with a brace or splint. For some injuries, such as a torn tendon, surgery may be considered.
Torn Ligaments and Muscles
Torn Ligaments and Muscles
Orthopaedic Treatments for Torn Ligaments and Muscles
Orthopaedic Treatments required for Sprain is an injury caused due to Torn Ligaments and Muscles.
Ligaments are bands of tissue that help connect bones, joints and organs and hold them in place. Ligaments are like cords made of connective tissue, elastic fibers that are somewhat stretchy, and collagen, a protein that binds tissues together. A ligament can be overstretched or torn is a common injury. Torn Ligaments and Muscles also called as Sprain.
Shreya Hospital at Ghaziabad is the best treatment center for Torn Ligaments and Muscles. Orthopedic Specialists working here have the expertise and experience to deal with such injuries perfectly. There diagnosis and treatment procedure is satisfactory as observed from patient feedback.
Ligaments have several important jobs that help you move properly:
- Allow the joint to move in the direction(s) it was meant to move.
- Hold bones together.
- Make sure that joints don’t twist.
- Stabilize muscles and bones.
- Strengthen joints.
- Prevent bones from dislocating.
For example, your knee has four ligaments that keep it from moving side to side or backward. Ligaments also hold the uterus in place in a woman’s pelvis. Additionally, they connect the liver, intestine and stomach and hold them in place.
Causes of Torn Ligaments and Muscles
A ligament can be stretched or torn. This injury is called a sprain. It occurs when a ligament is forced to move in the wrong direction or stretches too far. Sprains often happen during a sudden fall, twist or impact.
Ligament injuries are common, especially in the:
- Ankle, knee or wrist.
- Back.
- Neck.
- Thumb or finger.
For example, if you step on a sidewalk curb the wrong way, you may twist and sprain your ankle. If you fall but catch yourself on an outstretched hand, you can injure the ligaments in your wrist. People sometimes injure ligaments from impact during a car or bike accident.
Symptoms of Torn Ligaments and Muscles
If you injure a ligament, symptoms may include:
- Bruising.
- Loose feeling in the joint.
- Pain.
- Popping or snapping sound.
- Swelling.
- Trouble bearing weight on the affected limb.
- Weakness in the joint.
An Orthopedic Specialist will grade your Torn Ligament by finding out how severe it is and what symptoms you have:
- Grade 1: A grade 1 sprain is a ligament that is overstretched or slightly torn. With a grade 1 strain, you’ll have minimal pain, swelling and bruising. You won’t have much trouble putting weight on that part of the body or using it.
- Grade 2: A grade 2 sprain involves a partial ligament tear. Signs include bruising, swelling, some pain and some difficulty using the body part or putting weight on it.
- Grade 3: A grade 3 sprain is a complete ligament tear or rupture. It causes severe bruising, swelling and pain. With a grade 3 sprain, you cannot use or put weight on that part of the body.
Diagnosis
Doctor might go through one or more from bellow procedure while diagnosing your injury:
- Ask you about your symptoms and when they started.
- Conduct a physical exam by looking at the injured area and assessing how it moves.
- Order imaging tests if necessary, such as MRI, to take pictures of the ligament.
- Take X-rays to rule out a broken bone or other problem.
Orthopaedic Treatments
Treatments for ligament injuries vary greatly, depending on:
- How long you’ve had symptoms.
- How severe the injury is (grade 1, 2 or 3).
- Whether it’s interfering with your life.
Treatment may range from:
- RICE: Rest, Ice, Compression (with an elastic bandage) and Elevation.
- Nonsteroidal anti-inflammatory drugs (NSAIDs).
- Immobilization (such as a splint, sling or brace) or assistive devices (for example, crutches to keep weight off the injury).
- Physical therapy.
- Surgery.
Knee Pain
Knee Pain
Orthopaedic Treatments for Knee Pain

The severity of Knee Pain may vary, depending on the cause of the problem.
Knee pain is a common problem that affects people of all ages. Knee pain may be the result of an injury, such as a ruptured ligament or torn cartilage. Medical conditions including arthritis, gout and infections also can cause knee pain.
Many types of minor knee pain respond well to self-care measures. Physical therapy and knee braces also can help relieve pain. In some cases, however, your knee may require surgical repair.
Symptoms of Knee Pain
The severity of knee pain may vary, depending on the cause of the problem. Signs and symptoms that sometimes accompany knee pain include:
- Swelling and stiffness
- Redness and warmth to the touch
- Weakness or instability
- Popping or crunching noises
- Inability to fully straighten the knee
Causes of Knee Pain
Knee pain can be caused by injuries, mechanical problems, types of arthritis and other problems.
A knee injury can affect any of the ligaments, tendons or fluid-filled sacs (bursae) that surround your knee joint as well as the bones, cartilage and ligaments that form the joint itself. Some of the more common knee injuries include:
- ACL injury. An ACL injury is a tear of the anterior cruciate ligament (ACL) — one of four ligaments that connect your shinbone to your thighbone. An ACL injury is particularly common in people who play basketball, soccer or other sports that require sudden changes in direction.
- Fractures. The bones of the knee, including the kneecap (patella), can be broken during falls or auto accidents. Also, people whose bones have been weakened by osteoporosis can sometimes sustain a knee fracture simply by stepping wrong.
- Torn meniscus. The meniscus is the tough, rubbery cartilage that acts as a shock absorber between your shinbone and thighbone. It can be torn if you suddenly twist your knee while bearing weight on it.
- Knee bursitis. Some knee injuries cause inflammation in the bursae, the small sacs of fluid that cushion the outside of your knee joint so that tendons and ligaments glide smoothly over the joint.
- Patellar tendinitis. Tendinitis causes irritation and inflammation of one or more tendons — the thick, fibrous tissues that attach muscles to bones. This inflammation can happen when there’s an injury to the patellar tendon, which runs from the kneecap (patella) to the shinbone and allows you to kick, run and jump. Runners, skiers, cyclists, and those involved in jumping sports and activities may develop patellar tendinitis.
Mechanical problems
Some examples of mechanical problems that can cause knee pain include:
- Loose body. Sometimes injury or degeneration of bone or cartilage can cause a piece of bone or cartilage to break off and float in the joint space. This may not create any problems unless the loose body interferes with knee joint movement, in which case the effect is something like a pencil caught in a door hinge.
- Iliotibial band syndrome. This occurs when the tough band of tissue that extends from the outside of your hip to the outside of your knee (iliotibial band) becomes so tight that it rubs against the outer portion of your thighbone. Distance runners and cyclists are especially susceptible to iliotibial band syndrome.
- Dislocated kneecap. This occurs when the triangular bone that covers the front of your knee (patella) slips out of place, usually to the outside of your knee. In some cases, the kneecap may stay displaced and you’ll be able to see the dislocation.
- Hip or foot pain. If you have hip or foot pain, you may change the way you walk to spare your painful joint. But this altered gait can place more stress on your knee joint and cause knee pain.
Types of arthritis
Some type of Arthritis most likely to affect the knee include:
- Osteoarthritis
- Rheumatoid arthritis
- Gout
- Pseudogout
- Septic arthritis
Other problems
Patellofemoral pain syndrome is a general term that refers to pain arising between the kneecap and the underlying thighbone. It’s common in athletes; in young adults, especially those whose kneecap doesn’t track properly in its groove; and in older adults, who usually develop the condition as a result of arthritis of the kneecap.
Risk factors
Many factors can increase your risk of having knee problems, include:
- Excess weight. Being overweight or obese increases stress on your knee joints, even during ordinary activities such as walking or going up and down stairs. It also puts you at increased risk of osteoarthritis by accelerating the breakdown of joint cartilage.
- Lack of muscle flexibility or strength. A lack of strength and flexibility can increase the risk of knee injuries. Strong muscles help stabilize and protect your joints, and muscle flexibility can help you achieve full range of motion.
- Certain sports or occupations. Some sports put greater stress on your knees than do others. Alpine skiing with its rigid ski boots and potential for falls, basketball’s jumps and pivots, and the repeated pounding your knees take when you run or jog all increase your risk of knee injury. Jobs that require repetitive stress on the knees such as construction or farming also can increase your risk.
- Previous injury. Having a previous knee injury makes it more likely that you’ll injure your knee again.
Prevention of Knee Pain
Following suggestions may help you to reduce chances of Knee Pain:
- Keep extra pounds off. Maintain a healthy weight; it’s one of the best things you can do for your knees. Every extra pound puts additional strain on your joints, increasing the risk of injuries and osteoarthritis.
- Be in shape to play your sport. To prepare your muscles for the demands of sports participation, take time for conditioning.
- Practice perfectly. Make sure the technique and movement patterns you use in your sports or activity are the best they can be. Lessons from a professional can be very helpful.
- Get strong, stay flexible. Weak muscles are a leading cause of knee injuries. You’ll benefit from building up your quadriceps and hamstrings, the muscles on the front and back of your thighs that help support your knees. Balance and stability training helps the muscles around your knees work together more effectively.And because tight muscles also can contribute to injury, stretching is important. Try to include flexibility exercises in your workouts.
- Be smart about exercise. If you have osteoarthritis, chronic knee pain or recurring injuries, you may need to change the way you exercise. Consider switching to swimming, water aerobics or other low-impact activities — at least for a few days a week. Sometimes simply limiting high-impact activities will provide relief.
Diagnosis
During the physical exam, Orthopedic Specialist might do:
- Inspect your knee for swelling, pain, tenderness, warmth and visible bruising
- Check to see how far you can move your lower leg in different directions
- Push on or pull the joint to evaluate the integrity of the structures in your knee
Imaging Tests
In some cases, your doctor might suggest tests such as:
- X-ray
- Computerized tomography (CT) scan
- Ultrasound
- Magnetic resonance imaging (MRI)
Lab tests
If your doctor suspects an infection or inflammation, you’re likely to have blood tests and sometimes a procedure called arthrocentesis, in which a small amount of fluid is removed from within your knee joint with a needle and sent to a laboratory for analysis.
Orthopaedic Treatments of Knee Pain
Orthopedic Specialist at Shreya Hospital, Ghaziabad have expertise in treating your Knee Pain. Treatments will vary, depending upon the exact cause of your knee pain.
Medications
Your doctor may prescribe medications to help relieve pain and to treat the conditions causing your knee pain, such as rheumatoid arthritis or gout.
Therapy
Strengthening the muscles around your knee will make it more stable. Your doctor may recommend physical therapy or different types of strengthening exercises based on the specific condition that is causing your pain.
If you are physically active or practice a sport, you may need exercises to correct movement patterns that may be affecting your knees and to establish good technique during your sport or activity. Exercises to improve your flexibility and balance also are important.
Arch supports, sometimes with wedges on one side of the heel, can help shift pressure away from the side of the knee most affected by osteoarthritis. In certain conditions, different types of braces may be used to help protect and support the knee joint.
Injections
In some cases, an Orthopedic Surgeon may suggest injecting medications or other substances directly into your joint. Examples include:
- Corticosteroids. Injections of a corticosteroid drug into your knee joint may help reduce the symptoms of an arthritis flare and provide pain relief that may last a few months. These injections aren’t effective in all cases.
- Hyaluronic acid. A thick fluid, similar to the fluid that naturally lubricates joints, hyaluronic acid can be injected into your knee to improve mobility and ease pain. Although study results have been mixed about the effectiveness of this treatment, relief from one or a series of shots may last as long as six months.
- Platelet-rich plasma (PRP). PRP contains a concentration of many different growth factors that appear to reduce inflammation and promote healing. Some studies have found that PRP may benefit certain people with osteoarthritis, but more studies are needed.
Surgery
If you have an injury that may require surgery, it’s usually not necessary to have the operation immediately. Before making a decision, consider the pros and cons of both nonsurgical rehabilitation and surgical reconstruction in relation to what’s most important to you. If you choose to have surgery, your options may include:
- Arthroscopic surgery. Depending on your injury, your doctor may be able to examine and repair your joint damage using a fiber-optic camera and long, narrow tools inserted through just a few small incisions around your knee. Arthroscopy may be used to remove loose bodies from your knee joint, remove or repair damaged cartilage (especially if it is causing your knee to lock), and reconstruct torn ligaments.
- Partial knee replacement surgery. In this procedure, your surgeon replaces only the most damaged portion of your knee with parts made of metal and plastic. The surgery can usually be performed through small incisions, so you’re likely to heal more quickly than you are with surgery to replace your entire knee.
- Total knee replacement. In this procedure, your surgeon cuts away damaged bone and cartilage from your thighbone, shinbone and kneecap, and replaces it with an artificial joint made of metal alloys, high-grade plastics and polymers.
- Osteotomy. This procedure involves removing bone from the thighbone or shinbone to better align the knee and relieve arthritis pain. This surgery may help you delay or avoid total knee replacement surgery.
Frozen Shoulder
Frozen Shoulder
Orthopaedic Treatments for Frozen Shoulder
Frozen Shoulder (adhesive capsulitis)
Frozen shoulder occurs when the capsule thickens and tightens around the shoulder joint, restricting its movement.
Frozen Shoulder means stiffness and pain in the shoulder joint. Symptoms generally begin slowly, then get worse. Over time, symptoms get better, usually within 1 to 3 years.
Having to keep a shoulder still for a long period increases the risk of developing frozen shoulder. This might happen after having surgery or breaking an arm. It’s usual for frozen shoulder to recur in the same shoulder. But some people can develop it in the other shoulder, usually within five years.
Treatment for frozen shoulder involves range-of-motion exercises. Sometimes treatment involves corticosteroids and numbing medications injected into the joint. Rarely, arthroscopic surgery is needed to loosen the joint capsule so that it can move more freely.
Shreya Hospital at Ghaziabad is popular in providing best solution for Frozen Shoulder. Orthopedic Surgeon working here with expertise can help you to reduce the symptoms and can guide you well enough to prevent recurrence of the disease.
Symptoms
Frozen shoulder typically develops slowly in three stages.
- Freezing stage. Any movement of the shoulder causes pain, and the shoulder’s ability to move becomes limited. This stage lasts from 2 to 9 months.
- Frozen stage. Pain might lessen during this stage. However, the shoulder becomes stiffer. Using it becomes more difficult. This stage lasts from 4 to 12 months.
- Thawing stage. The shoulder’s ability to move begins to improve. This stage lasts from 5 to 24 months.
For some people, the pain worsens at night, sometimes disrupting sleep.
Causes of Frozen shoulder
The shoulder joint is enclosed in a capsule of connective tissue. Frozen shoulder occurs when the capsule thickens and tightens around the shoulder joint, restricting its movement.
There is no specific reason, why this happens to some people. But it’s more likely to happen after keeping a shoulder still for a long period, such as after surgery or an arm fracture.
Risk factors
Certain factors may increase the risk of developing frozen shoulder.
Age and sex
People 40 and older, particularly women, are more likely to have frozen shoulder.
Immobility or reduced mobility
People who’ve had to keep a shoulder somewhat still are at higher risk of developing frozen shoulder. Restricted movement can be the result of many factors, including:
- Rotator cuff injury
- Broken arm
- Stroke
- Recovery from surgery
People who have certain diseases appear more likely to develop frozen shoulder. Diseases that might increase risk include:
- Diabetes
- Overactive thyroid (hyperthyroidism)
- Underactive thyroid (hypothyroidism)
- Cardiovascular disease
- Parkinson’s disease
Diagnosis
During the physical exam, a Specialist might ask you to move your arm in certain ways. This is to check for pain and see how far you can move your arm (active range of motion). Then you might be asked to relax your muscles while the provider moves your arm (passive range of motion). Frozen shoulder affects both active and passive range of motion.
Frozen shoulder can usually be diagnosed from signs and symptoms alone. But imaging tests — such as X-rays, ultrasound or MRI — can rule out other problems.
Orthopaedic Treatments
The procedure fallowed by Orthopedic Specialists at Shreya Hospital for frozen shoulder treatment mostly involves controlling shoulder pain and preserving as much range of motion in the shoulder as possible.
Medications
Pain relievers such as aspirin and ibuprofen (Advil, Motrin IB, others) can help reduce pain and inflammation associated with frozen shoulder. In some cases, a health care provider might prescribe stronger pain-relieving and anti-inflammatory drugs.
Therapy
A physical therapist can teach you range-of-motion exercises to help recover your shoulder movement. Your commitment to doing these exercises is necessary to regain as much movement as possible.
Surgical and other procedures
Most frozen shoulders get better on their own with time. For severe or persistent symptoms, other treatments include:
- Steroid injections. Injecting corticosteroids into the shoulder joint might help decrease pain and improve shoulder mobility, especially if given soon after frozen shoulder begins.
- Hydrodilatation. Injecting sterile water into the joint capsule can help stretch the tissue and make it easier to move the joint. This is sometimes combined with a steroid injection.
- Shoulder manipulation. This procedure involves a medication called a general anesthetic, so you’ll be unconscious and feel no pain. Then the care provider moves the shoulder joint in different directions to help loosen the tightened tissue.
- Surgery. Surgery for frozen shoulder is rare. But if nothing else helps, surgery can remove scar tissue from inside the shoulder joint. This surgery usually involves making small incisions for small instruments guided by a tiny camera inside the joint (arthroscopy).
Sports Injuries
Sports Injuries
Orthopaedic Treatments for Sports Injuries
A sports injury can be acute (sudden) or chronic (develop over time).
Sports injuries are common and can occur throughout your body to bones, muscles, tendons, ligaments and other structures. Exercise is important to good health, but people often get hurt when participating in sports or other physical activities. A sports injury involves damage to part of your body due to sports, exercise or athletic activities.
Sports injuries can happen to anyone, particularly people who:
- Are out of shape.
- Don’t wear proper protective equipment.
- Exercise without warming up and cooling down.
- Participate in contact sports that may involve tackling or collisions.
- Take part in activities that involve jumping, running and pivoting or changing direction quickly.
Body parts mostly affected due to Sports Injuries are:
- Achilles tendon: The Achilles tendon is a thick cord that connects the back of your lower leg (calf) to your heel. It helps you walk. But the tendon can become swollen, inflamed and stiff. It can even tear. This is called Achilles tendinitis or Achilles tendon rupture.
- Ankle: Your leg and foot join together at your ankle. It contains three joints, as well as several bones, cartilage, ligaments, muscles and tendons. Ankle pain is often caused by a sprained ankle.
- Elbow: Your elbow is the joint that acts as a hinge between your upper and lower arm. People often experience pain in their elbow from repeat motions and overuse (for example, tennis elbow and Little League elbow).
- Head: Your head includes your face, skull and brain. One of the most common head injuries is concussion.
- Knee: Your knee is a complex joint that acts as a hinge between your thigh and lower leg. It contains bones, cartilage, ligaments and tendons. Knee pain can be caused by jumper’s knee or runner’s knee. Other common injuries include meniscus tear and anterior cruciate ligament (ACL) tear.
- Shoulder: Your shoulder connects your upper arm to the trunk of your body. It contains your rotator cuff, a group of muscles and tendons that keep the upper arm in your shoulder socket. Rotator cuff tendinitis and rotator cuff tears are common sports injuries.
The most common sports injuries are:
- Broken bone: A broken bone (bone fracture) can happen when sudden force is applied to a bone.
- Cartilage tear: Cartilage is a tough but flexible shock absorber that covers and protects the ends of some bones. Cartilage injuries can occur in joints such as your knee and shoulder.
- Concussion: A concussion is a brain injury caused by a bump or blow to your head.
- Dislocation: Dislocation occurs when the end of a bone moves out of its normal position in a joint. For example, if your shoulder pops out of its socket, it’s dislocated.
- Tendinitis: Tendinitis occurs when your tissues that connect muscles to bones (tendons) become swollen and inflamed. It’s caused by repetitive movements over time. An example is jumper’s knee (patellar tendonitis).
- Sprains: A sprain happens when a ligament stretches too much or tears. Ligaments connect bones and stabilize joints. These injuries can be mild or severe, and they’re common in your ankle, knee and wrist.
- Strains: A strain occurs when you overextend a muscle and it stretches or tears. Examples include hamstring strain, back strain and abdominal strain.
Causes of Sports Injuries
- Accidents, such as a fall.
- Bad habits with exercise, such as not warming up or stretching enough.
- Lack of safety equipment, or gear that’s damaged or worn incorrectly.
- Shoes that don’t fit well or provide enough support.
- Sudden start to an exercise program or significant increase in physical activity that your body isn’t used to.
Symptoms of Sports Injuries
- Aches, pain or tenderness.
- Bruising.
- Deformity, such as a bone or joint looking out of place.
- Decreased range of motion.
- Grinding, cracking, clicking or popping noise.
- Inability to bear weight on your hip, leg or foot.
- Skin that’s warm to the touch.
- Stiffness or weakness.
- Swelling.
- Trouble moving a body part normally (for example, you can’t move it as far or it locks up when you try to move).
Diagnosis
Shreya Hospital at Ghaziabad is the best treatment center for Sports Injuries. Orthopedic Specialists practicing here have vast experience and expertise in treating any kind of Sports Injuries.
To diagnose a sports injury, our Orthopedic Specialist performs a physical exam. They’ll ask questions about what happened and what symptoms you’ve had. They’ll also look at the injured area, possibly testing how it moves.
Depending on the type of injury you have and how severe it is, your healthcare provider also may recommend imaging tests. An X-ray, CT scan or MRI can create pictures of the structures inside your body. The images will help your healthcare provider understand, diagnose and treat your specific injury.
Orthopaedic Treatments
Treatment for sports injuries varies widely, depending on the type and severity. Many sports injuries heal in a few days or weeks with rest and at-home strategies.
But for more serious injuries, treatment may involve:
- Immobilization with a cast, splint, sling, walking boot or other medical device.
- Injections to reduce swelling and pain.
- Prescription anti-inflammatory medications.
- Surgery to correct fractures or repair ligament, tendon or cartilage tears.
- Physical therapy (also called rehabilitation or rehab) to heal and strengthen injured body parts.
Bunions, Foot, Ankle Injuries
Bunions, Foot, Ankle Injuries
Orthopaedic Treatments for Bunions, Foot, Ankle Injuries

Bunions on the big toe are the most common
A bunion is a bump that forms on the outside of the big toe. This foot deformity occurs from years of pressure on the big toe joint (the metatarsophalangeal, or MTP, joint). Eventually, the toe joint gets out of alignment, and a bony bump forms. The medical term for bunions is hallux abducto valgus. Bunions can form on one or both feet. Shreya Hospital in Ghaziabad provides best treatment for relieving symptoms of Bunions. Though it doesn’t vanish completely, still you will get relief from symptoms and be able to do your daily work comfortably.
Bunions on the big toe are the most common. Other types include:
- Congenital hallux valgus: Some babies are born with bunions.
- Juvenile or adolescent hallux valgus: Tweens and teens between the ages of 10 and 15 may develop bunions.
- Tailor’s bunion: Also called a bunionette, this bunion forms on the outside base of the little (pinky) toe.
Causes of Bunions:
- Pressure from the way you walk (foot mechanics)
- shape of your foot (foot structure) causes your big toe to bend in toward the second toe.
- Family history of bunions due to inherited foot structure problems, like flatfeet.
- Foot injuries
- Inflammatory diseases, such as rheumatoid arthritis.
Signs and Symptoms:
- A bunion resembles a turnip — red and swollen.
- Inability to bend the big toe, or pain and burning when you try to bend it.
- Difficulty wearing regular shoes.
- Corns or calluses (thickened skin).
- Hammertoes (painful, tight toe tendons and joints).
- Numbness in the big toe.
Diagnosis:
- Specialist can diagnose a bunion by looking at it.
- X-rays to check for joint damage and bone alignment.
Orthopaedic Treatments
Bunions don’t go away. Treatment help relieving symptoms and may include:
- Bunion pads and taping: Over-the-counter bunion pads can cushion the area and ease pain. You can also use medical tape to keep the foot in the correct position.
- Footwear changes: Switching to shoes with wide, deep toe boxes can take pressure off of your toes. You may be able to use a stretching device to widen shoes you already own.
- Orthotic devices: Over-the-counter or custom-made shoe inserts (orthotics) can help to control alignment issues such as pronation that may be contributing to bunion formation. You can also place a spacer between the big toe and second digit. Some people find relief by wearing a splint at night to keep the big toe straight.
- Pain relievers: Nonsteroidal anti-inflammatory drugs (NSAIDs) both oral and topical can be combined with ice packs help with pain and swelling.
- Physical therapy: Massage, physical therapy and ultrasound therapy can break up soft-tissue adhesions to reduce pain and inflammation. There are actually exercises that can help improve muscle strength around the bunion and can modestly improve alignment.
- Injections: Steroid injections may reduce pain and swelling but may also be damaging if used too often or injected into the joint itself. This is often a late treatment of bunions when trying to avoid surgery.
- Surgery: If nonsurgical treatments don’t help, and walking becomes extremely painful, your provider may recommend surgery. This procedure is called a bunionectomy. Your provider removes the bunion and realigns bones to bring the big toe back into the correct position.
Bone Tumors
Bone Tumors
Orthopaedic Treatments for Bone Tumors
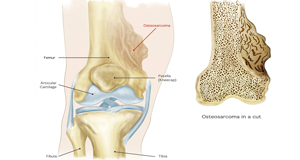
Benign Bone Tumors are Non Cancerous
Bone Tumors means an abnormal growth of cells within a bone. Bone Tumors may be Cancerous (Malignant) or Non-Cancerous (Benign). In fact, non-cancerous bone tumors are much more common than cancerous ones.
Shreya Hospital in Ghaziabad is the best treatment center of Bone Tumors. Dr.Dev Mishra, Senior Orthopaedic Surgeon is having vast experience of Orthopaedic Treatments and Orthopaedic Surgeries. Operation Theater having advance equipment and Dedicated Team of Orthopaedic Specialists result in successful treatment of Bone Tumors.
Benign Bone Tumors
Benign Bone Tumors are Non-Cancerous. These tumors may cause pain that gets worse and not better. Some benign bone tumors may need treatment to stop them from destroying bone. Other non-cancerous bone tumors may require no treatment at all.
Risk Factors:
Most Bone Tumors that start in your bones are benign (not cancer). This means that benign tumors will not spread from their original site to a new location. Bone Tumors can form in any of the bones of your skeletal system and in any part of the bone. In general, the most common bones involved are also some of the largest: the femur, tibia, humerus, pelvis, spine and ribs. Some types of tumors are most common in specific locations, such as the spine or near the growth plates in your hip, knee or shoulder.
Benign Bone Tumors are most common in people who are under 30 years old. A large portion of Benign Bone Tumors are found in children while their skeletons are still growing.
The most common Types of Benign Bone Tumors include:
- Enchondroma: This type of tumor starts in the cartilage. These tumors are found inside the bone, in the marrow space.
- Osteochondroma: This type of tumor is made up of cartilage and bone and can get bigger while the skeleton is growing. These tumors grow outside the bone.
- Non-ossifying fibroma: This bone tumor is the most common bone tumor found in children. They often go away on their own and are most commonly discovered incidentally on X-rays after an injury.
- Chondroblastoma: This type of tumor is usually removed because its growth affects nearby joints. It’s found in children and can cause significant pain.
- Osteoid osteoma: This type of tumor usually affects the long bones of the body and is more common in males. It can cause significant pain at nighttime due to hormone interaction and can be relieved with nonsteroidal anti-inflammatory medications (NSAIDs).
- Osteoblastoma: This type of tumor is also more common in males. Treatment is almost always surgery.
- Periosteal chondroma: These tumors are made up of cartilage and are located on the surface of a bone. Treatment is almost always surgery.
- Giant cell tumor: These tumors, though rare, grow aggressively. Females are slightly more likely to develop giant cell tumors. Treatment is almost always surgery.
- Chondromyxoid fibroma: This very rare type of tumor begins in the bone marrow. Treatment is almost always surgery.
- Aneurysmal bone cyst (ABC): These tumors can grow very large. Treatment with repeated injections of a sclerotherapy medication or with surgery is commonly needed. The sclerotherapy medication helps the space fill in.
- Unicameral [simple] bone cysts (UBC): These tumors are generally found near growth plates and are often found when they weaken the bone enough to cause a fracture. Treatment is usually surgery to do a bone graft or add a sclerotherapy medication.
- Fibrous dysplasia: This is a common bone tumor that shows up as a single bone tumor or multiple bone tumors. Generally, it doesn’t need surgery unless the bone becomes weakened by the size of the tumor.
Cancerous Bone Tumors
Cancers that start in the bones are called primary bone tumors. Bone cancers that start in another part of the body (such as the breast, lungs, or colon) are called secondary or metastatic bone tumors. They behave very differently from primary bone tumors.
Cancerous primary bone tumors include:
- Chondrosarcoma
- Ewing sarcoma
- Fibrosarcoma
- Osteosarcomas
Cancers that most often spread to the bone are cancers of the:
- Breast
- Kidney
- Lung
- Prostate
- Thyroid
These forms of cancer usually affect older people.
Causes require Orthopaedic Treatments
There is no specific cause of bone tumors. They often occur in areas of the bone that grow rapidly. Possible causes include:
- Genetic defects passed down through families(Hereditary)
- Radiation
- Injury
Diagnosis:
Doctor will start diagnosis from a complete physical examination and if required can ask you for tests. Imaging tests can help determine the location and size of bone tumors. It also helps to find out whether the tumors have spread to other parts of the body or not. The types of imaging tests recommended depend on your individual signs and symptoms. One or more tests might required include:
- Bone Scan
- X-Rays
- CT Scan
- MRI Scan
- Biopsy
Orthopaedic Treatments
Treatment of bone tumors is dependent on the type of tumor. Where available, people with bone tumors are treated at Shreya Hospital, Ghaziabad, the best Bone Tumors Treatment Centre which have surgeons, radiologists, pathologists, oncologists and other support staff. Generally, noncancerous bone tumors may be observed for changes and surgery offered if there is pain or pressure effects on neighbouring body parts. Surgical resection with or without cytotoxic drugs may be considered.
Chemotherapy and radiotherapy
Chemotherapy and radiotherapy are effective in some tumors (such as Ewing’s sarcoma) but less so in others (such as chondrosarcoma). There is a variety of chemotherapy treatment protocols for bone tumors. The protocol with the best-reported survival in children and adults is an intra-arterial protocol where tumor response is tracked by serial arteriogram. When tumor response has reached >90% necrosis surgical intervention is planned.
Medication
One of the major concerns is bone density and bone loss. Non-hormonal bisphosphonates increase bone strength and are available as once-a-week prescription pills. Strontium-89 chloride is an intravenous medication given to help with the pain and can be given in three-month intervals.
Surgical treatment
Treatment for some bone cancers may involve surgery, such as limb amputation, or limb sparing surgery (often in combination with chemotherapy and radiation therapy). Limb sparing surgery, or limb salvage surgery, means the limb is spared from amputation.
Instead of amputation, the affected bone is removed and replaced in one of two ways:
- Bone graft, in which bone is taken from elsewhere on the body or
- Artificial bone is put in. In upper leg surgeries, limb salvage prostheses are available.
There are other joint preservation surgical reconstruction options, including allograft, tumor-devitalized autograft, vascularized fibula graft, distraction osteogenesis, and custom-made implants. An analysis of massive knee replacements after resection of primary bone tumours showed patients did not score as highly on the Musculoskeletal Tumour Society Score and Knee Society Score as patients who had undergone intra-articular resection.
Thermal ablation techniques
Over the past two decades, CT guided radiofrequency ablation has emerged as a less invasive alternative to surgical resection in the care of benign bone tumors, most notably osteoid osteomas. In this technique, which can be performed under conscious sedation, a RF probe is introduced into the tumor nidus through a cannulated needle under CT guidance and heat is applied locally to destroy tumor cells.
While initial success rates with RFA are high, symptom recurrence after RFA treatment has been reported, with some studies demonstrating a recurrence rate similar to that of surgical treatment.
Thermal ablation techniques are also increasingly being used in the palliative treatment of painful metastatic bone disease. Currently, external beam radiation therapy is the standard of care for patients with localized bone pain due to metastatic disease. Although the majority of patients experience complete or partial relief of pain following radiation therapy, the effect is not immediate and has been shown in some studies to be transient in more than half of patients.
For patients who are not eligible or do not respond to traditional therapies ( i.e. radiation therapy, chemotherapy, palliative surgery, bisphosphonates or analgesic medications), thermal ablation techniques have been explored as alternatives for pain reduction.
These studies are limited however to patients with one or two metastatic sites; pain from multiple tumors can be difficult to localize for directed therapy. More recently, cryoablation has also been explored as a potentially effective alternative as the area of destruction created by this technique can be monitored more effectively by CT than RFA, a potential advantage when treating tumors adjacent to critical structures.
Bursitis
Bursitis
Orthopaedic Treatments for Bursitis

Bursitis often occurs near joints that perform frequent repetitive motion.
Bursitis is a painful condition that affects the small, fluid-filled sacs that is called bursae, that cushion the bones, tendons and muscles near your joints. Bursitis occurs when bursae become inflamed.
The most common locations for bursitis are in the shoulder, elbow and hip. But you can also have bursitis by your knee, heel and the base of your big toe. Bursitis often occurs near joints that perform frequent repetitive motion.
Symptoms
If you have bursitis, the affected joint might:
- Feel achy or stiff
- Hurt more when you move it or press on it
- Look swollen and red
Causes of Bursitis require Orthopaedic Treatments
The most common causes of bursitis are repetitive motions or positions that put pressure on the bursae around a joint. Which include:
- Throwing a baseball or lifting something over your head repeatedly
- Leaning on your elbows for long periods
- Extensive kneeling for tasks such as laying carpet or scrubbing floors
Other causes include injury or trauma to the affected area, inflammatory arthritis such as rheumatoid arthritis, gout and infection.
Risk factors
Anyone can develop bursitis, factors can increase your risk include:
- Age. Bursitis becomes more common with aging.
- Occupations or hobbies. If your work or hobby requires repetitive motion or pressure on particular bursae, your risk of developing bursitis increases. Examples include carpet laying, tile setting, gardening, painting and playing a musical instrument.
- Other medical conditions. Certain systemic diseases and conditions — such as rheumatoid arthritis, gout and diabetes — increase your risk of developing bursitis. Being overweight can increase your risk of developing hip and knee bursitis.
Prevention of Bursitis
Not all types of bursitis can be prevented, but you can reduce risk and the severity of flare-ups by changing the way you do daily tasks.
- Using kneeling pads. Use some type of padding to reduce the pressure on your knees if your job or hobby requires a lot of kneeling.
- Lifting properly. Bend your knees when you lift. Failing to do so puts extra stress on the bursae in your hips.
- Wheeling heavy loads. Carrying heavy loads puts stress on the bursae in your shoulders. Use a dolly or a wheeled cart instead.
- Taking frequent breaks. Alternate repetitive tasks with rest or other activities.
- Maintaining a healthy weight. Being overweight places more stress on your joints.
- Exercising. Strengthening your muscles can help protect your affected joint.
- Warming up and stretching before strenuous activities to protect your joints from injury.
Diagnosis
Shreya Hospital at Ghaziabad is the best treatment center for Bursitis. Orthopedic Specialists practicing here have expertise and vast experience in treating Bursitis.
They diagnose bursitis based on a medical history and physical exam. If required, might ask for bellow tests:
- Imaging tests. X-ray images can’t positively establish the diagnosis of bursitis, but they can help to exclude other causes of your discomfort. Ultrasound or MRI might be used if your bursitis can’t easily be diagnosed by a physical exam alone.
- Lab tests. Your doctor might order blood tests or an analysis of fluid from the inflamed bursa to pinpoint the cause of your joint inflammation and pain.
Orthopaedic Treatments
Bursitis generally gets better on its own. Conservative measures, such as rest, ice and taking a pain reliever, can relieve discomfort. If it don’t work, Doctor might suggest:
- Medication. If the inflammation in your bursa is caused by an infection, your doctor might prescribe an antibiotic.
- Therapy. Physical therapy or exercises can strengthen the muscles in the affected area to ease pain and prevent recurrence.
- Injections. A corticosteroid drug injected into the bursa can relieve pain and inflammation in your shoulder or hip. This treatment generally works quickly and, in many cases, one injection is all you need.
- Assistive device. Temporary use of a walking cane or other device will help relieve pressure on the affected area.
- Surgery. Sometimes an inflamed bursa must be surgically drained, but only rarely is surgical removal of the affected bursa necessary.
Joint Pain
Joint Pain
Orthopaedic Treatments for Joint Pain

Age is also a factor responsible for Joint Pain.
Joint Pain is usually felt in the hands, feet, hips, knees, or spine. Pain may be constant or it can come and go. Sometimes the joint can feel stiff, achy, or sore. Some patients complain of a burning, throbbing, or “grating” sensation. In addition, the joint may feel stiff in the morning but loosen up and feel better with movement and activity. However, too much activity could make the pain worse.
Joint pain may affect the function of the joint, and can limit a person’s ability to do basic tasks. Severe joint pain can affect the quality of life. Treatment should focus not only on pain but also on the affected activities and functions.
Orthopedic Specialists at Shreya Hospital, Ghaziabad are efficient enough to give you relief from Severe Joint Pain. Joint Pain, very common problem found almost in all age groups is diagnosed and treated carefully.
Joint pain is more likely to affects those who:
- Have had previous injuries to a joint
- Repeatedly use and/or overuse a muscle
- Have arthritis or other chronic medical conditions
- Suffer from depression, anxiety, and/or stress
- Are overweight
- Suffer from poor health
Age is also a factor in stiff and painful joints. After years of use, and wear and tear on joints, problems may arise in middle-aged or older adults.
Causes of Joint Pain require Orthopaedic Treatments
The most common causes of pain in joints are:
- Osteoarthritis, a common type of arthritis, happens over time when the cartilage, the protective cushion in between the bones, wears away. The joints become painful and stiff. Osteoarthritis develops slowly and usually occurs during middle age.
- Rheumatoid arthritis is a chronic disease that causes swelling and pain in the joints. Often the joints become deformed (usually occurring in the fingers and wrists).
- Gout is a painful condition where crystals from the body collect in the joint, causing severe pain and swelling. This usually occurs in the big toe.
- Bursitis is caused by overuse. It is usually found in the hip, knee, elbow, or shoulder.
- Viral infections, rash, or fever may make joint movement painful.
- Injuries, such as broken bones or sprains
- Tendinitis is an inflammation of the tendons, or the flexible bands that connect bone and muscle. It is typically seen in the elbow, heel, or shoulder and is usually caused by overuse.
Orthopaedic Treatments
Sometimes the pain may go away by taking over-the-counter medication, or by performing simple daily exercises. Other times, the pain may be signaling problems that can only be corrected with prescription medication or surgery.
- Simple at-home treatments, such as applying a heating pad or ice on the affected area, may be recommended for short periods, several times a day. Soaking in a warm bathtub may also offer relief.
- Exercise can help get back strength and function. Walking, swimming, or other low-impact aerobic exercise is best. Those who participate in strenuous workouts or sports activities may need to scale it back or begin a low-impact workout routine. Gentle stretching exercises will also help. Check with the doctor before beginning or continuing any exercise program.
- Weight loss may also be suggested, if needed, to lessen strain on joints.
- Acetaminophen, (Tylenol®) or anti-inflammatory drugs (ibuprofen), may help ease the pain. Both of these medicines are available over the counter, but stronger doses may need a doctor’s prescription. If you have a history of stomach ulcers, kidney disease, or liver disease, check with your physician to see if this is a good option for you.
- Topical treatments, such as ointments or gels that can be rubbed into the skin over the affected joint area, may also help ease pain. Some of these may be found over the counter, or the doctor may write a prescription.
- Dietary supplements, like glucosamine, may help relieve pain. Ask the doctor before taking any over-the-counter supplements.
If those medications or treatments do not ease the pain, the doctor may prescribe:
- Supportive aids, such as a brace, cane, or orthotic device in the shoe, can help support the joint to allow ease of movement. The doctor, physical or occupational therapist, or social worker will be able to assist with the right option(s) available.
- Physical or Occupational Therapy, along with a balanced fitness program, may gradually help ease pain and improve flexibility.
- Antidepressants may be prescribed to help improve sleep for a patient suffering from joint pain.
- Steroids, often given by injection into the joint, provide short-term relief of pain and swelling.
- Painkilling drugs that help ease pain.
Surgery
Surgery may be an option if the joint pain is long lasting and does not lessen with drugs or physical therapy and exercise. Please be sure to discuss this with the doctor to make sure that an operation makes sense.
There are many different surgical options available, including:
Arthroscopy: A procedure where a surgeon makes two or three small incisions in the flesh over the joint and gets into the joint using an arthroscope, or a thin, flexible, fiberoptic instrument, to repair cartilage or remove bone chips in or near the joint.
Joint replacement: If other treatments do not help, surgery may be needed to replace the joint once the cartilage that cushions and protects the ends of the bones gradually wears away. This can be done for hip, knee and shoulder joints.
A surgeon removes parts of the patient’s bone and implants an artificial joint made from metal or plastic. This procedure has had excellent results and the majority of patients feel long-lasting pain relief after this type of surgery.
 Dr Dev Mishra Best Orthopaedic Doctor in Delhi NCR Ghaziabad
Dr Dev Mishra Best Orthopaedic Doctor in Delhi NCR Ghaziabad